Genetics vs Environment, Determining Mental Illness
Jerry Liu - University of Waterloo
With one in five adults suffering from a diagnosable mental disorder (National Alliance on Mental Illness [NAMI], 2015), it is one of the most common problems in our modern society. To make matters worse, the number has been increasing over the past decade and is not showing signs of slowing down (Befrienders Worldwide, n.d.). It is reported that the average high school student has similar anxiety to the average psychiatric patient in the 1950s (Leahy, 2008). Scientists have long questioned the root cause of these conditions and while technology continues to help society gain a better understanding of different diseases, there has been little advancement towards mental health. Although technological advancements in drug creation have provided treatment medication for mental disorders, their current effectiveness is marginally better than a placebo because there is little understanding of the conditions the drug is being used on (Insel, 2011). However, recent research has been done on the genetic origins of mental disorders (National Institutes of Health [NIH], 2013). In this report, I discuss some potential genetic and environmental factors that influence mental illness. With the latest developments in gene engineering and gene modification, we may be at the forefront of revolutionary treatment.
Numerous studies have claimed to identify some of the leading genes behind mental illness. It has become well known that disorders including autism, bipolar disorder, ADHD, major depressive disorder and schizophrenia tend to run in families (NIH, 2013), which suggests genetic origin. Delving deeper, an international research consortium scanned thousands of genetic markers in over 33, 000 patients, who each had at least one of the five aforementioned illnesses, and compared them to a group of 28, 000 people with no major psychiatric diagnosis (NIH, 2013). Analysis revealed variations were significantly associated with all five of the disorders; specifically, in two genes that code for calcium flow into neurons. One of these genes, CACNA1C, was previously linked to bipolar disorder, schizophrenia and major depression. It is known to affect emotion, thinking, attention and memory. Furthermore, a region on chromosome 3 had disorder-linked variation to all five conditions. This study marked the first extensive comparison between people with and without a mental illness, thus more research is required before the results can be claimed conclusive. However, other studies have been inconclusive. For example, the Evaluation of Genomic Applications in Practice and Prevention Working Group (EGAPP Working Group) published a hypothesis on the link between CYP450 genes and depression, hoping to assist clinicians with prescribing of anti-depressants (Centers for Disease Control and Prevention [CDC], 2011). Despite extensive tests and clinical trials, there was a lack of strong evidence and the group could not come to a conclusion on the relationship between the genome and depression. These studies provide evidence on the impact genes have when predicting mental illness, but also indicate that other factors such as the environment are involved too.
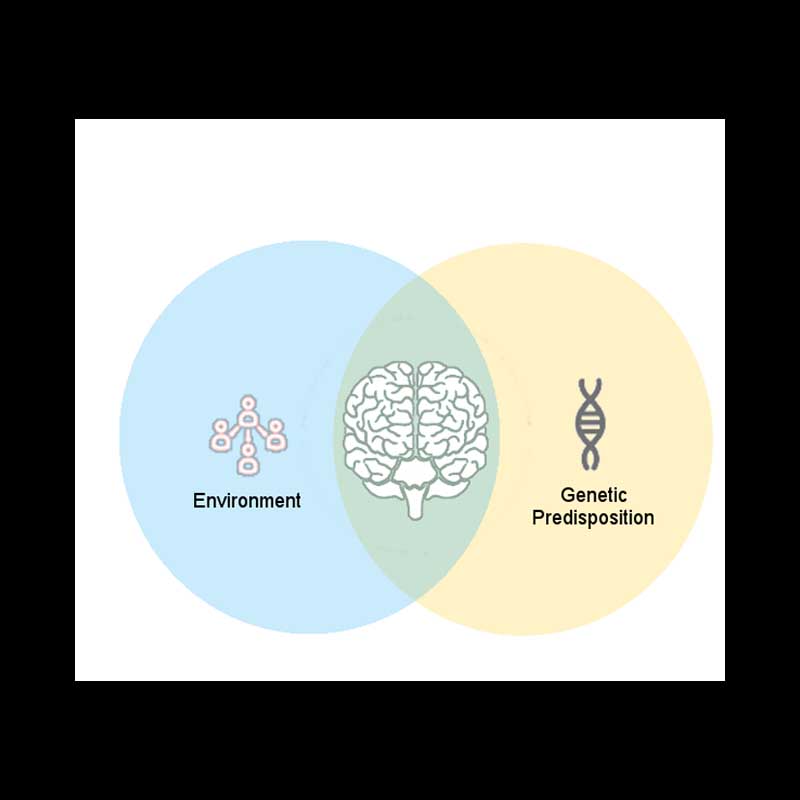
Environmental factors may also play an important role in the development of mental illness. Interestingly, the drastic increase in anxiety does not match the change in the human genome of the past half-century. Using the definition of environment as everything but the inherited gene, given by Schmidt (2007), it encompasses all factors beyond genetics. Breaking “environment” down, it could refer to anything from drugs to injury to nutrition. To describe the potential effects of the environment, Professor Ronald Kessler from Harvard Medical School stated: “Feelings of pure loss might lead to depressive disorders, while feelings of pure danger might lead to anxiety disorders, and feelings of loss and danger might lead to both simultaneously.” To test these theories, scientists often study identical twins due to their shared DNA. In one study, by Charles Schmidt, they found that when one twin became schizophrenic, the other had a less than 50% chance of developing the same condition (2007). This suggests environmental factors are significant factors behind mental illness, causing two humans with nearly identical genes to develop differently. After determining that there is evidence for both genetic and environmental factors on mental illness, the scientists aimed to study the connection between them.
Past research has shown promising evidence that genetic and environmental factors are much more intertwined than previously thought. A study in 2002 found that the maltreatment of a child would mutate the MAOA gene, which is responsible for neurotransmitters in the brain, thus potentially causing the child to develop an antisocial personality disorder (Schmidt, 2007). While this may seem negative at first, this also demonstrates the potential to change how a child will act when they grow up. For example, a child who may be naturally violent could become more docile (Schmidt, 2007). The following year, it was discovered that young people who undergo emotionally stressful situations are at a higher risk of depression if they have the serotonin transporter gene (Schmidt, 2007). Moreover, this gene was also related to heightened activity in the amygdala, which is responsible for processing fear. This heightened activity could cause daily activities to be perceived as more menacing (Schmidt, 2007). The research on environmental factors provides new insight into treatment possibilities. Rather than relying on state-of-the-art technology, changing the people and environment that a child grows up with could be more than enough to improve their state of mental health.
In conclusion, there is strong evidence on the factors influencing mental illness, both genetic and environmental. They are both determinants of mental health, but the effect of each one on the other has not been studied in detail. Due to the nature of these disorders, they are typically defined by thoughts and emotions, which vary depending on events and circumstances. This makes it more difficult to come to a conclusion compared to a tumour diagnosis, which is usually a binary yes/no. As research continues in this field, further analyses of the interconnected roles of genes and the environment will provide the foundation for more successful treatments of mental disorders.
References
National Alliance on Mental Illness. (2015, October 23). Mental Health By The Numbers. http://www.nami.org/Learn-More/Mental-Health-By-the-Numbers
Befrienders Worldwide (n.d.). Suicide Statistics. http://www.befrienders.org/suicide-statistics
Leahy, R. (2008, April 30). Antidepressants: A complicated picture. https://www.nimh.nih.gov/about/directors/thomas-insel/blog/2011/antidepressants-a-complicated-picture.shtml
National Institutes of Health. (2013, March 18). Common Genetic Factors Found in 5 Mental Disorders. https://www.nih.gov/news-events/nih-research-matters/common-genetic-factors-found-5-mental-disorders
Centers for Disease Control and Prevention. (2011, January 20). Mental Health Awareness. https://www.cdc.gov/genomics/resources/diseases/mental.html
Schmidt, C. (2007, Aug). Environmental Connections: A Deeper Look into Mental Illness https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1940091/
